What is Rapamycin? From Easter Island Discovery to Longevity Medicine
A Remarkable Discovery Hidden in the Soil of a Remote Island
In 1964, a fascinating scientific expedition set sail from Halifax, Nova Scotia, aboard the HMCS Cape Scott. The Medical Expedition to Easter Island brought together approximately 40 doctors and scientists with an ambitious goal—to study the health and genetics of one of the world’s most isolated populations before the Chilean government disrupted their seclusion with a new airport.
Among the expedition members was Georges Nógrády, a microbiologist from the University of Montreal. Nógrády wasn’t searching for miracle drugs when he methodically divided Easter Island into 67 sections and collected soil samples from each. He was investigating a medical mystery: why didn’t the island’s inhabitants suffer from tetanus despite walking barefoot everywhere, even though horses—common carriers of tetanus bacteria—outnumbered the island’s population?
What Nógrády discovered in those soil samples would launch a billion-dollar pharmaceutical industry and fundamentally change our understanding of aging biology. Within one sample lived a bacterium called Streptomyces hygroscopicus that produced an unknown compound. This molecule, eventually named rapamycin after the island’s native name Rapa Nui, would become one of the most significant discoveries in modern medicine.
What is Rapamycin and How Does It Work?
Rapamycin is a macrolide compound with immunosuppressive and antiproliferative properties, first isolated from bacterial samples collected on Easter Island in 1964. The compound works by inhibiting a critical cellular protein complex called mTOR—an acronym that literally stands for “mechanistic (or mammalian) target of rapamycin.”
Understanding the mTOR Pathway
The mTOR pathway is an evolutionarily conserved metabolic signaling cascade that regulates cell division, growth, and survival, integrating signals from growth factors, nutrients, and energy status to control protein synthesis, lipid metabolism, and autophagy.
Think of mTOR as your body’s master growth regulator. When you eat, mTOR activity increases, signaling cells to grow, divide, and produce proteins. When you stop eating or fast, mTOR activity slows down, and your cells shift into maintenance and repair mode through a process called autophagy—essentially cellular housekeeping where damaged components get cleared away.
The mTOR pathway acts as a master regulator of cell growth, integrating signals from growth factors, nutrients, and energy status to control several important cellular processes including protein synthesis, lipid metabolism, and autophagy.
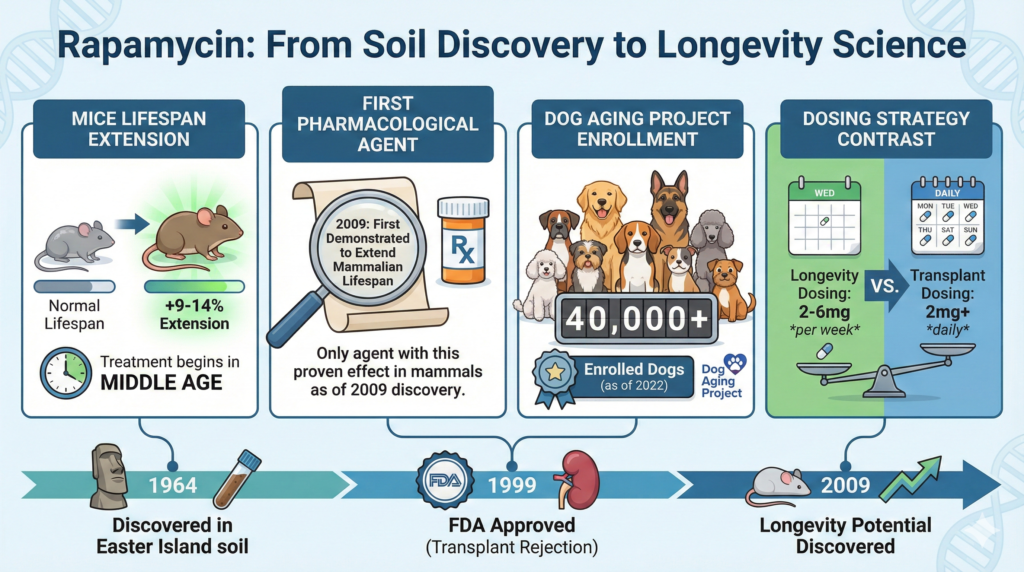
FIGURE-1: Key Information for Rapamycin
From Antifungal to Anti-Aging: Rapamycin’s Scientific Journey
The Path to FDA Approval
The soil samples Nógrády collected sat largely forgotten until 1969, when they were given to scientists at Ayerst Pharmaceuticals in Montreal. Within those vials lived a bacterium with the ability to produce rapamycin, initially valued as the strongest antifungal agent ever discovered, with effectiveness against Candida species greater than the potent drug amphotericin B.
Dr. Surendra Sehgal at Ayerst discovered that rapamycin also had antiproliferative activity—it could stop cells from multiplying. When Ayerst consolidated its workforce and closed the Montreal research facility, Sehgal took samples of the bacterium home and placed them in his freezer, where they stayed until Ayerst and Wyeth merged in 1988. This dedication preserved what would become a breakthrough medication.
In 1999, the US Food and Drug Administration approved rapamycin as an immunosuppressant under the brand name Rapamune (sirolimus), primarily used to prevent organ transplant rejection.
The Longevity Breakthrough
The discovery that would transform rapamycin from transplant drug to potential anti-aging therapy came in 2009. David Harrison, Randy Strong and Richard Miller, leading a team of 13 American scientists, found that rapamycin could extend the lifespans of mice by 9-14%, even when treatment began at 20 months old—the equivalent in mouse years of a 60-year-old human.
This finding was revolutionary. Rapamycin became the only known pharmacological treatment that increases lifespan in all model organisms studied, from yeast to worms, flies, and mammals.
How Rapamycin Affects Aging: The Science Explained
The Hyperactivity of mTOR and Aging
Research demonstrates that mTOR pathway activity is elevated in many tissues with age and correlates with a decline in clearance of damaged proteins and organelles, while hyperactive mTOR signaling has been implicated in many age-related conditions including cancer, type 2 diabetes, and neurodegeneration.
David Sabatini, a scientist at the Whitehead Institute who discovered mTOR in the mid-1990s, explains that lots of things go wrong with aging, and the only way to impact many of those things is by affecting a pathway that’s a master regulator. We’re unlikely to find just one thing that mTOR does to impact aging—the reason mTOR inhibition works is because it affects multiple cellular processes simultaneously.
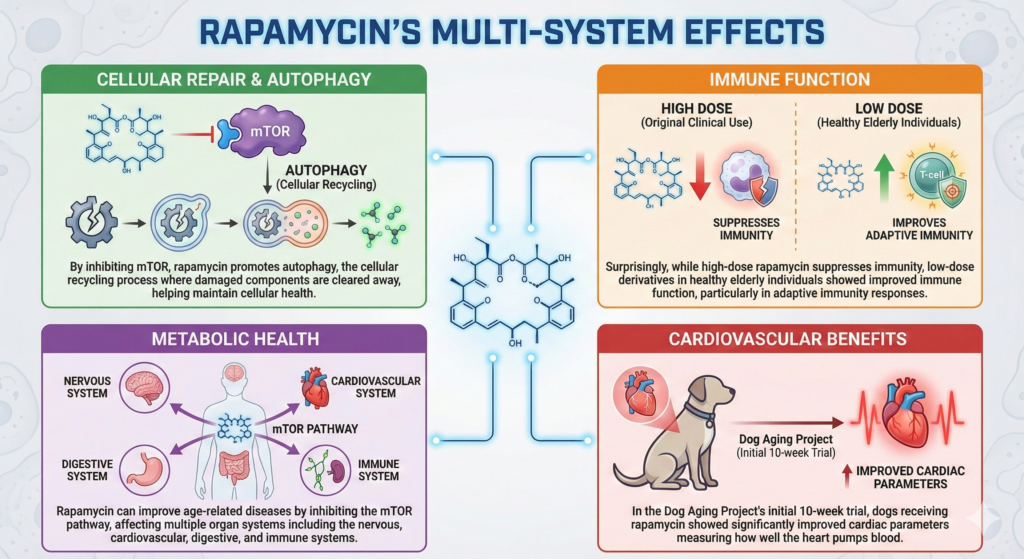
FIGURE-2: Rapamycin’s Multi-System Effects
Leading Researchers on Rapamycin for Longevity
Dr. Matt Kaeberlein and the Dog Aging Project
Dr. Matt Kaeberlein, Professor at the University of Washington, founded the Dog Aging Project to demonstrate that companion dogs can provide a compelling model for aging and age-related disease, with rapamycin being the most robust and reproducible drug for impacting both longevity and healthspan in complex animals.
The Dog Aging Project represents a unique approach to longevity research. As of 2022, nearly 40,000 dogs have been registered, with the majority participating in a 10-year longitudinal study, while approximately 500 dogs are enrolled in a double-blind, placebo-controlled study of rapamycin called TRIAD (Test of Rapamycin in Aging Dogs).
Why dogs? The biological aging process is very similar in dogs and people—one piece of evidence is that dogs get many of the same age-related diseases as humans, they just happen seven times faster. This means longevity studies that would take decades with humans can be completed in a few years.
Dr. Peter Attia’s Perspective on Rapamycin
Dr. Peter Attia, the popular physician and best-selling author, classifies rapamycin as “promising” rather than proven, noting that while the Interventions Testing Program confirms rapamycin’s potential to prolong lifespan in mice, there isn’t enough human data to support its pro-longevity effects in humans.
Attia has publicly stated he has been taking rapamycin for several years and prescribes it to fewer than 10% of his patients under controlled protocols, emphasizing that intermittent dosing may be safer and more effective than chronic use.
VIDEO-1: What is Rapamycin? dr. Peter Attia Explains
What Are the Side Effects and Risks of Rapamycin?
Understanding rapamycin’s side effects requires recognizing an important distinction: the side effects observed in transplant patients taking high daily doses differ significantly from what’s emerging in low-dose, intermittent protocols for longevity.
Side Effects at Transplant Doses
Common side effects of rapamycin in transplant patients include mouth sores, headaches, joint pain, increased cholesterol and triglycerides, decreased kidney function, increased infection risk, impaired wound healing, and potential effects on blood cell counts.
In a retrospective study of 219 kidney transplant patients taking rapamycin, 98% experienced at least one side effect, with the most common being dyslipidemia (52%), peripheral edema (37%), cytopenia (36%), and acne (29%).
Low-Dose Rapamycin for Longevity
The dosing of rapamycin for anti-aging purposes is a fraction of the dose used for transplant patients—typically 2-6 mg per week in a single dose rather than daily dosing, and there have not been any studies demonstrating severe side effects at these small pulsatile doses.
A 2024 systematic review found that no serious adverse events attributed to rapamycin and its derivatives were reported in healthy individuals, though there were increased numbers of infections and increases in total cholesterol and LDL cholesterol.
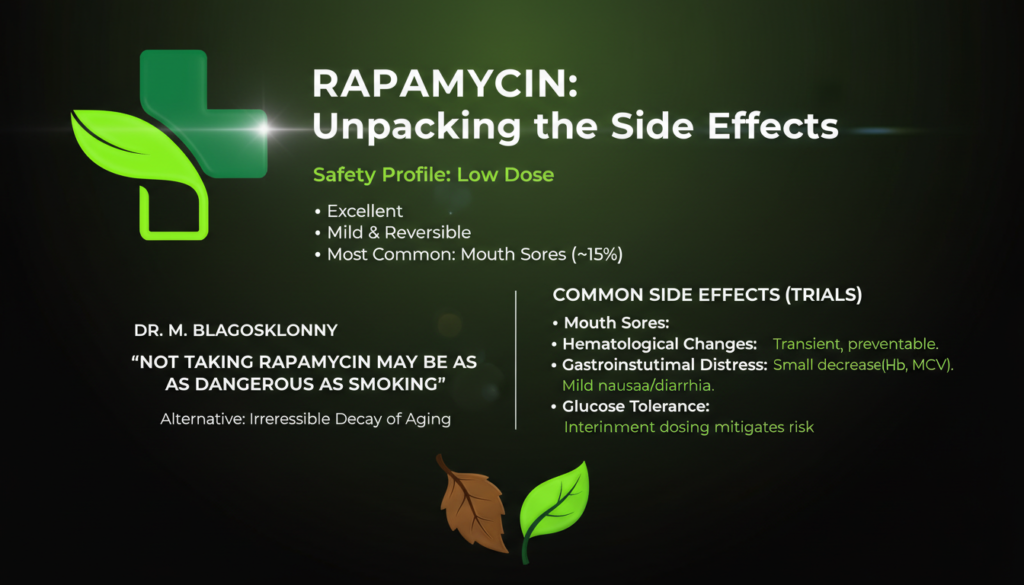
FIGURE-3: Safety Profile and Major Side Effects of Low Dose Rapamycin
Important Warnings
Who Should Not Take Rapamycin:
- Pregnant or breastfeeding women
- People with active infections or immune deficiencies
- Individuals with severe liver disease
- Those scheduled for surgery (should be discontinued beforehand)
- People with known allergies to rapamycin
Drug Interactions: Rapamycin interacts with numerous medications including certain antibiotics, antifungals, and notably grapefruit juice, which can dangerously increase rapamycin levels.

Recent Human Studies: What Does the Research Show?
The PEARL Trial Results (2024-2025)
The PEARL trial (Participatory Evaluation of Aging with Rapamycin for Longevity) represents one of the largest and longest randomized control trials testing rapamycin for healthy human aging, with 114 participants completing the 48-week study receiving either 5 mg/week, 10 mg/week of rapamycin, or placebo.
The PEARL trial showed rapamycin was generally well-tolerated at low doses, with some improvements in subjective wellbeing measures. However, the review of current evidence found no clear clinical evidence that rapamycin extends life or clearly slows the aging process in humans, pointing to the urgent need for larger, better-designed human trials.
Oxford Study on Immune Function (2025)
A new study from Oxford University found that older adults taking 1 mg/day of rapamycin for 8 weeks showed reduced markers of cell senescence in immune cells, with 60% of immune cells surviving DNA damage compared to only 20% in untreated cells.
The Bottom Line on Human Evidence
Despite the preclinical evidence supporting rapamycin to enhance lifespan in animals, the data in humans have yet to establish that rapamycin or its analogues is a proven senotherapeutic that can delay aging in healthy older adults.
Where Can You Get Rapamycin? Availability and Options
Prescription Requirements
Rapamycin is not available as an over-the-counter supplement. As a potent pharmaceutical regulated by the FDA, rapamycin requires a doctor’s prescription and must be administered under careful medical supervision.
Online Longevity Clinics
Several telemedicine services now offer rapamycin prescriptions specifically for longevity purposes. Services include a consultation, acquiring a prescription, and subscription to the prescribed dose. Alternatively blood tests are offered.
Over The Counter
Medical Grade Rapamycin is available over the counter in India, and individuals from the US, CA, UK & AU can import a 90 day supply of prescription drugs for personal use by policy.
This option does not necessarily require a prescription, and individuals should schedule their consecutive blood tests if desired. Over the counter options are 30 to 50% of the cost of prescribed, and therefore attracting a lot of attention from the biohacker community. However, due to growing demand to Rapamycin, reputable suppliers are hard to find among the crowd.

The Ethical Complexity: Rapamycin’s Origins
The story of rapamycin raises important ethical questions. The discovery of rapamycin on Rapa Nui set the foundation for all subsequent research and commercialization, yet the Rapa Nui people have received little to no acknowledgment or monetary benefit from this billion-dollar drug.
Many individuals have used rapamycin to gain fame, financial success, and clinical triumph, all of whom owe gratitude to the Rapanui, yet the Rapanui have not shared in the wealth that has come from the discovery of this compound.
This history serves as a reminder that scientific progress often has complex origins, and recognition of indigenous contributions to medical discoveries remains an ongoing discussion.
The Future of Rapamycin Research
Ongoing Clinical Trials
Multiple trials are currently investigating rapamycin and its derivatives:
- Expanded Dog Aging Project TRIAD trials with larger cohorts
- Human trials examining specific age-related conditions
- Studies testing combination therapies (such as rapamycin with trametinib)
- Research on tissue-specific effects and optimal dosing regimens
Unanswered Questions
Critical questions remain about the frequency and dosing of rapamycin use in humans, with experts emphasizing reservations about indiscriminately prescribing rapamycin as a longevity drug without more data.
Key unknowns include:
- Optimal dosing schedules for longevity (daily vs. weekly vs. intermittent)
- Long-term safety in healthy aging populations
- Tissue-specific effects and biomarkers
- Individual variation in response
- Interaction with exercise and diet interventions
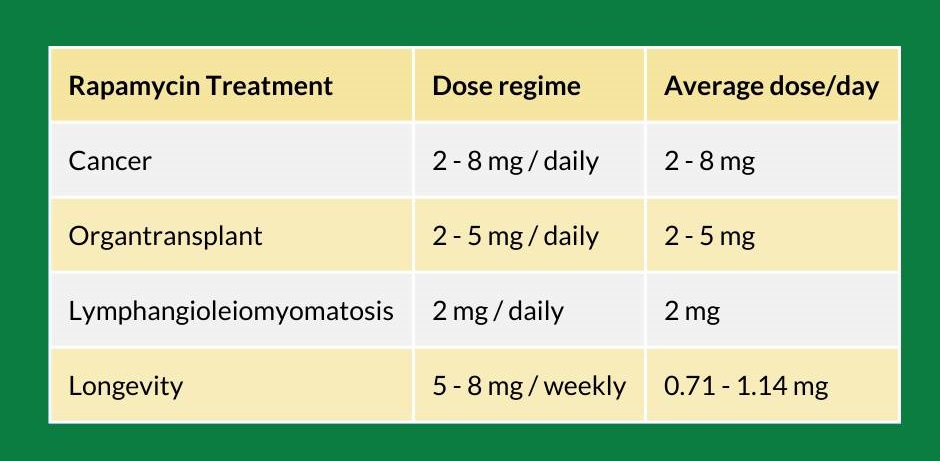
TABLE-1: Rapamycin Dosing for Different Treatments
Key Takeaways
Rapamycin’s journey from Easter Island soil to potential longevity medicine is remarkable, but the story is far from complete:
- Proven in Animals: Rapamycin administration initiated in mid-life extends lifespan by 9-14% in mice and is associated with delayed onset of age-related pathologies.
- Human Evidence Limited: While promising signals exist in human trials, definitive proof of life extension or slowing aging in humans remains elusive.
- Prescription Required: Rapamycin is a powerful pharmaceutical requiring medical supervision, not a casual anti-aging supplement.
- Individual Approach Needed: Anyone considering rapamycin should work with knowledgeable healthcare providers, undergo regular monitoring, and have realistic expectations.
- Research Continues: Ongoing trials will provide crucial data about safety, efficacy, and optimal protocols for healthy aging.
Conclusion: A Promising but Uncertain Path Forward
Rapamycin represents one of the most exciting developments in longevity science. Its ability to extend lifespan across diverse species—from yeast to mammals—combined with a growing understanding of the mTOR pathway’s central role in aging, makes it a compelling candidate for human healthspan extension.
However, enthusiasm must be tempered with scientific rigor. The translation from mouse to human remains uncertain, and the long-term effects of mTOR inhibition in healthy humans are still unknown. As the research community continues to unravel rapamycin’s potential, the compound serves as both a testament to serendipitous discovery and a reminder of the complexity of human aging biology.
For those considering rapamycin, the path forward should involve thorough medical consultation, realistic expectations, careful monitoring, and an understanding that we’re still in the early chapters of this remarkable compound’s story.